In this in-depth article Spotlight delves into the drivers of heroin use in the country, the policies that could help curb it, and those that could make it even worse.
Between 215,000 and 425,000 people were using heroin daily across South Africa in 2020 (at the upper limit, this amounts to more than 1% of the country’s entire adult population). This is according to a study published recently in the Journal of Illicit Economies and Development, which also finds that somewhere between 78,000kg to 155,000kg of the drug was consumed that year (the equivalent of about one to two A320 Airbus jets used by SAA).
Even if we rely on the lower figure, the research suggests that heroin use has ballooned over recent years as there were only about 110,000 people estimated to be using the drug in 2015. This lines up with the views of drug specialists who argue that heroin use shot up in the mid- to late 2010s.
To work out the new figures, researchers worked with people who use narcotics across nine major cities to map out areas where drug users congregate. Teams of researchers then visited these hotspots and interviewed users in order to work out the size of the illicit drug market in individual wards across each city. A panel of researchers then collated this data to approximate how much drug consumption was taking place across the country
Consequently, there is a fair amount of guesswork that goes into developing the figures. Yet, this is only one of several sources of data that shows that South Africa has a serious and growing heroin problem.
Take data from rehab facilities. The South African Community Epidemiology Network on Drug Use (Sacendu) includes a web of drug and alcohol treatment centres across South Africa. About 70% of all rehab facilities in the country are connected to the programme, according to the South African Medical Research Council (SAMRC), which runs the programme.
Data provided to Spotlight by the SAMRC shows that in 2012, about 12% of all people who came to Sacendu treatment sites were there primarily because of opioids – a class of drug that includes heroin and pain-relief medicines like codeine. A decade later, this had increased to almost 18%. Previous research shows that the majority of opioid-related admissions to Sacendu sites take place because of heroin specifically.
South Africa’s sewers also provide clues. When the body digests drugs like heroin, it produces particular substances called metabolites, which are excreted and serve as biological markers. Scientists snooping about in four wastewater treatment plants across Gauteng detected metabolites for heroin as well as a range of other opioids in the sewage at each plant.
Additionally, between 2002 and 2018, the South African Police Service dealt with an increasing number of heroin cases each year, while household surveys reveal that over roughly the same period, there was a sharp increase in the number of South Africans who admitted to recently taking opioids (Spotlight dissected these findings here).
Opioids are a category of drug which are either derived from the poppy plant or are developed in a laboratory to mimic its properties. These lab-made “synthetic opioids” include pain-relief drugs like oxycodone and fentanyl, which have played a central role in the opioid crisis in the US. South Africa has largely managed to steer clear of the synthetic opioid epidemic however, and although the country has faced a troubling rise in codeine misuse, scholars who spoke to Spotlight say heroin is the biggest driver of South Africa’s opioid crisis.
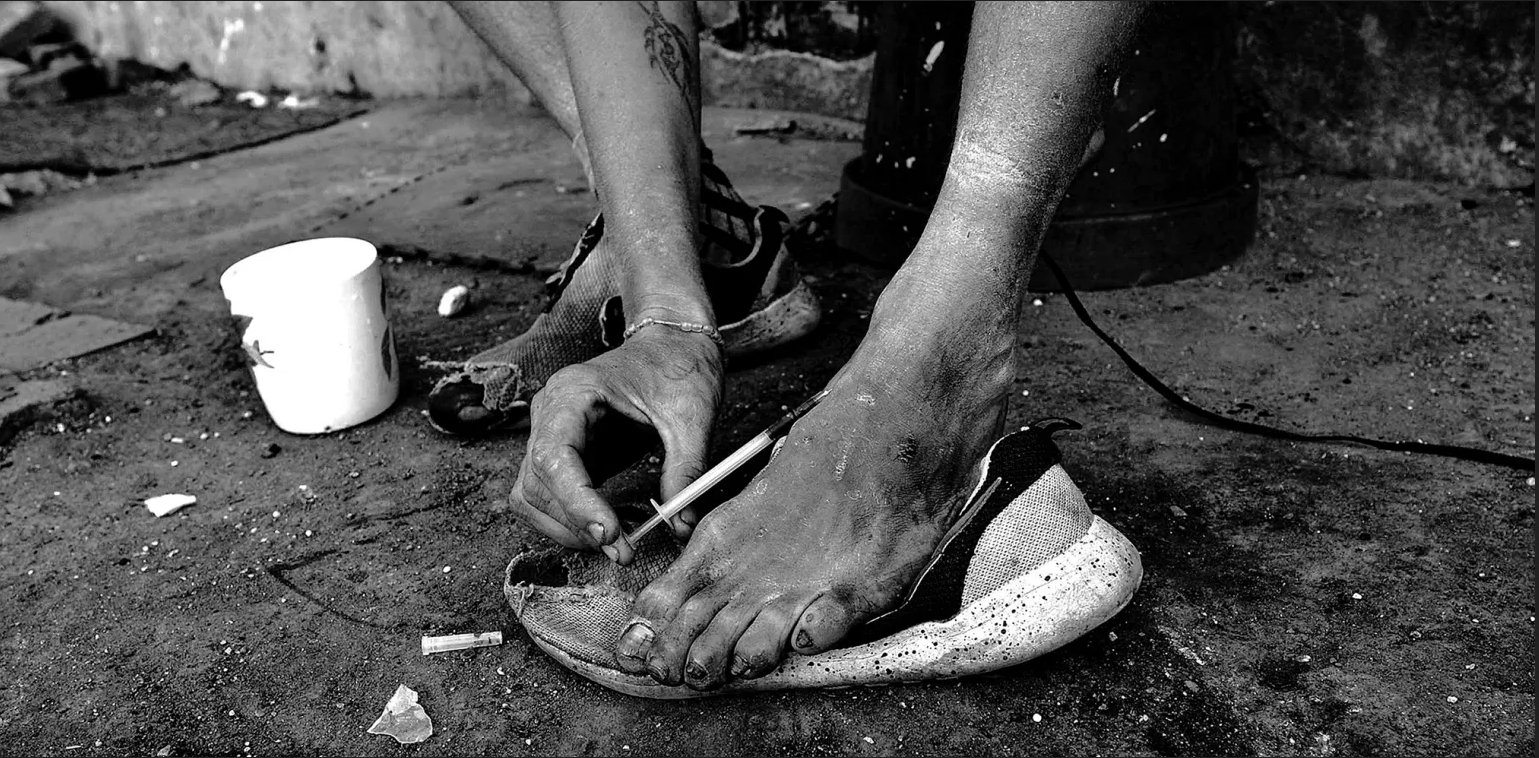
This has wide-ranging health effects. For instance, while treatment centres find that most heroin users in South Africa smoke the drug, a sizeable minority also inject it. Since contaminated needles are sometimes used and shared, such people face an increased risk of contracting blood-borne viruses like hepatitis C, which has already become widespread among users in some South African cities.
Researchers argue that the heroin epidemic is largely going unnoticed due in part to public narratives that have misrepresented the problem.
Narratives around ‘nyaope’ obscure the heroin crisis
“Nyaope,” “whoonga” and “sugars” are some of the names that have featured since about 2010 to describe a supposedly new drug stalking South Africa’s streets. It is often alleged to be a “cocktail substance” which combines heroin with rat poison, antiretrovirals (ARVs), concrete and a range of other scary-sounding ingredients to create a uniquely addictive mix.
Earlier this year, however, a laboratory analysis of nyaope samples obtained from the South African police found that for the most part the drug is just ordinary high-grade heroin. This supports an argument that has long been made by certain scholars, that media accounts that frame nyaope as a new and exotic drug are often misleading, and have obscured the fact that South Africa simply has a major heroin crisis.
How did nyaope/whoonga come to be seen as a unique drug? One explanation is that several other laboratory studies have found that some nyaope specimens contain substances other than heroin.
For instance, a 2016 paper found small amounts of an old ARV drug called zidovudine (which is no longer used in standard ARV treatment) in some of the nyaope that was tested. However, rather than making up a precise mixture, the presence of additives other than heroin varies across samples and studies. For instance, in the 2016 research, traces of zidovudine were only present in three out of 12 samples, while many other chemical analyses did not find any ARVs in the drug.
Additionally, researchers like the University of Pretoria’s Shaun Shelly told Spotlight that additives like zidovudine wouldn’t have been used to create a uniquely addictive drug. Instead, he argues they were “bulking agents” used to increase the volume of heroin sold, a practice that has also been identified in many Western countries.
Contaminated needles increase the risk of contracting blood-borne viruses like hepatitis C. (Photo: Nico Franz / Pixabay)
Working out exactly how to define nyaope nevertheless remains contentious. Some, like the SAMRC, refer to the drug as “low-grade heroin”, while others, like the authors of the new 2024 lab-based analysis, argue that it should simply “be considered synonymous with heroin”.
This is in line with a 2020 report by the Global Initiative Against Transnational Organised Crime, which found that drug dealers in South Africa make no distinction between heroin, nyaope and whoonga, and that the same product is being sold regardless of the title used.
The report also finds that while drug dealers have cut heroin/nyaope with bulking agents in the past, this practice is less common today (this may explain the contrast between the results of previous chemical studies and the recent 2024 paper). For instance, the report quotes a drug dealer in Johannesburg who states: “In the early days, we mixed heroin with other stuff to make the volume bigger, and you could do it because there wasn’t a lot of competition and a lot of people didn’t know anything purer; but those days are over, there’s a lot of heroin in the system and if you mix it, people won’t buy from you.”
How did the crisis get so bad?
Many researchers highlight South Africa’s social and economic malaise as contributing to the drug crisis, noting that in a context of soaring rates of depression and unemployment, heroin provides certain people with temporary relief. “Some will say to you [heroin] is like lying in the arms of my mother and lover at the same time… I feel at peace,” explains Shelly, who says the experience gives some people a sense that they can “protect themselves from the world”.
And people in South Africa face no shortage of hardships. Research shows that people in the country who face domestic abuse – which is widespread – are more likely to say that they had recently taken illicit substances.
Part of the crisis is also being driven by factors that are external to South Africa, such as the shift in international drug supply routes, which have made greater use of South Africa to get heroin from Afghanistan (where poppies are cultivated) to consumer markets in Europe and Asia. This has led to a large increase in the flow of heroin through South Africa’s borders, and while much of this is in transit, spin-off markets for local consumption were quickly generated, according to Enact, an EU-funded research project.
This spike in supply likely contributed to the fall in heroin prices during the 2000s and 2010s, meaning the drug became more accessible than ever. For instance, research in Cape Town found that in 2004, a gram of heroin/nyaope cost about R215 – a decade later, it had fallen to R119 (note these are just the nominal prices, when we consider inflation the decline is even more extreme).
More policing could backfire
Now that tonnes of the product is flowing into the country, trying to plug the supply through stricter border enforcement is unlikely to be effective, according to Dr Andrew Scheibe, a harm reduction researcher at the University of Pretoria.
A common consequence of increased border policing is a “balloon effect”, he argues. Much like pushing down on a balloon would only displace the air instead of eliminating it, monitoring of border posts more strictly just results in drugs entering through new routes.
“Even countries that have really good, well-resourced border controls still can’t control the [flood] of illicit drugs,” says Scheibe. Consider the US-Mexico border, for instance, or the huge amounts of illicit substances entering Europe.
If they can’t do it, then it’s unlikely that we would be successful, argues Scheibe, who highlights South Africa’s vast borderland as well as the “culture of corruption” that allows cartels to circumnavigate policing.
Many others agree. A policy brief by Enact states it’s unlikely that more border enforcement would yield success as “South Africa’s borders are large and current heroin routes, which primarily come through the Mozambican border, have much scope to shift”.
Even if the country were able to block the supply of heroin, this may have unintended consequences.
For instance, according to Shelly, it is partially because South Africa has a steady flow of heroin that we don’t face a fentanyl crisis like the one that has ravaged the US. In that country, more than 70,000 people died in 2021 due to overdoses on synthetic opioids (mainly fentanyl). These deaths frequently occur alongside other substances like heroin, partially because in the US powdered drugs are sometimes laced with fentanyl, which can increase the risk of overdose.
Shelly says that adulteration happens for financial reasons – the drug is more potent than heroin and therefore smaller amounts of it are required to get a user high. Consequently, it’s “much easier to get fentanyl across the border than heroin”. South Africa doesn’t face that problem, according to Shelly, who explains that “part of the reason is because heroin is cheap and easily available here… [so] there’s no financial incentive to cut another drug into it”.
Blocking the supply of heroin could change this calculus. In the absence of straightforward policing measures, public health tools offer one solution to reducing the harm.
Opioid substitution therapy needed
When a person takes heroin, the body quickly converts it into morphine, eliciting euphoric feelings. However, most of that morphine exits the body within a few hours, leaving people who are dependent on heroin with cravings for more. Such people usually need to take a dose “every four to six hours” and “if they don’t they go into withdrawal, which is very unpleasant”, according to Scheibe.
Indeed, Shelly explains that people who try to quit the drug often say that the withdrawal symptoms make them “feel like their life is ending”. In reality, it’s “the same as awful flu”, he notes, “but that does not discount the fact that it’s very difficult to overcome those feelings four to five times a day, or on a continual stretch, for a week, when you know you could just take [heroin] to take it away”.
It’s for this reason that a medically assisted route called opioid substitution therapy (OST) is a far more effective way to stop using heroin than simply going cold turkey. OST is a treatment option in which a person who is dependent on heroin can replace the drug with medically prescribed opioids such as methadone or buprenorphine. This is typically offered in combination with other forms of support such as therapy.
Scheibe explains that “from a very simplistic pharmacological perspective, what the methadone does [is that it] binds to the same receptor in the brain as heroin does, but it lasts longer, so you [usually] only need to take it once a day”.
Rather than getting the user high, methadone simply allows people to avoid withdrawals, he says, and because it stays in the body longer than heroin, people don’t have to constantly be thinking about their next fix. This “allows them to focus on other things in their life”, he says, which may include building relationships or managing a career.
This process takes time, however. “They will need the treatment for at least six months, sometimes it’s years, others will need it for life,” notes Scheibe, who adds that the duration depends on how long people had been taking heroin.
Clinical trials have repeatedly shown that rehabilitation programmes that rely on OST for at least six months are more effective than abstinence-based approaches. It’s therefore no surprise that South Africa’s Drug Master Plan states that OST is an “evidence-based intervention for individuals who are opiate dependent”.
Despite this, heroin users who rely on government services are largely unable to access medically assisted rehabilitation – at most they can get methadone for about a week, either at public hospitals or state-run rehab centres. An exception is an OST programme in Tshwane which is funded by the municipality.
One obstacle to increasing the roll-out of the drug is likely to be financial. In 2017, the Tshwane-based project spent about R2,400 per person to procure methadone at the recommended dose.
However, Scheibe notes that with enough political will, prices can always change. “[G]overnment is able to shape the market by using the tender mechanism,” he says, noting that the cost can be brought down through “procurement of large volumes of medication in a competitive manner”.
He also notes we could be using money the government is investing in abstinence-based programmes that are “not effective”. Indeed, research on state-run rehab centres in Johannesburg (where methadone is only offered in the first week of treatment) paints a grim picture.
Roughly five months after people were first initiated in rehabilitation, self-reported depression had skyrocketed (the opposite has occurred at small South African OST projects). Meanwhile, two-thirds of heroin users had gone back to the drug (though many were using less frequently). And among those who had stayed off heroin, some started using other illicit substances to cope – as a result, there were more people relying on crystal meth after treatment than at onset. DM
Stay informed with The Namibian – your source for credible journalism. Get in-depth reporting and opinions for
only N$85 a month. Invest in journalism, invest in democracy –
Subscribe Now!