THE co-infection of Tuberculosis (TB) and HIV-AIDS is causing havoc in the southern town of Keetmanshoop.
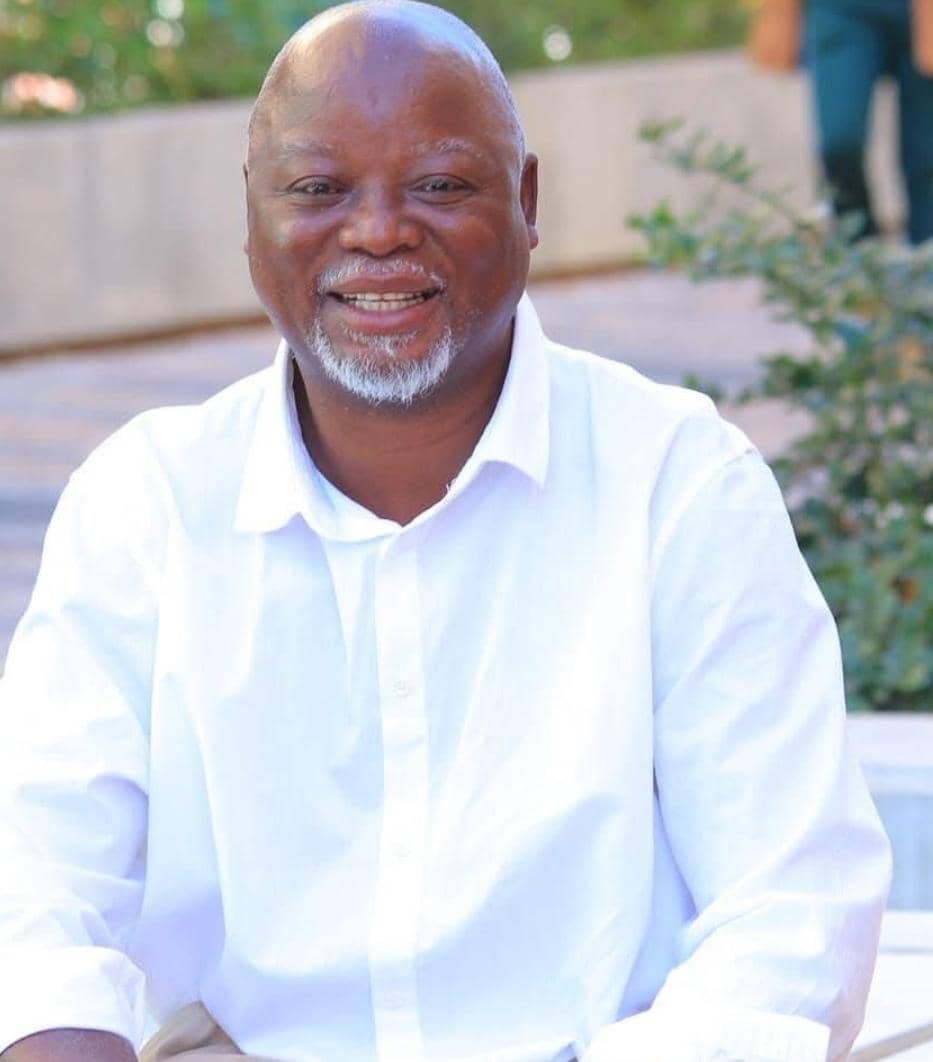
Health officials fear that it will be difficult to control the situation if people continue to stigmatise the two diseases. The diseases are the major causes of death people in the area face.Principal medical officer at the Keetmanshoop Hospital, Dr Emmanuel Dumebi Adigwe, said it was “just too difficult to control them”.In an interview with The Namibian, Adigwe said the issue was complicated by the dropout rate of those on TB treatment and the stigma that HIV-infected people face.”We are in pain over the defaulters.The dropout rate is worrying and the consequences are very harsh on the patients.They develop resistance,” he said.Statistics available from national TB campaigners indicate that the disease has not only became one of the two major causes of death but is responsible for a significant number of institutional deaths.When Namibia applied for funding from the Global Fund for AIDS, TB and Malaria, it indicated that 10 per cent of all deaths in Namibia were due to TB.Between 1991 and 2000, the rate of notification has risen from 430 for every 100 000 to 619/100 000 a year.The escalation is due to the link between the two diseases.Drug resistance has increased because some patients fail to follow prescribed schedules when taking their medicine.The Ministry has since introduced the Directly Observed Treatment, Short Course or DOTS strategy.Adigwe said defaulters were the most costly patients to treat and were spreading multi-drug resistant strains.Drug-resistant strains can cost up to N$25 000 to treat, as opposed to N$250 to treat a new infection.At best, only half of those infected with the new strains can be cured.If left untreated, one person can infect up to 15 others.The DOTS strategy relies on testing, monitoring and an uninterrupted supply of effective medicine.A person diagnosed with TB has to take medication every day for six months.For those who do not, TB can be deadly.Dr Adigwe said TB was worsened by the culture of sharing and the high rate of alcoholism in the region.”People drink at shebeens without eating.They tend to share one tombo container and if one has TB, it is likely to be spread.That is why Karas is one of the regions with the highest prevalence,” he said.Eventually, Dr Adigwe and his colleagues initiated a “food-for-TB” programme.”It was a local arrangement which was never blessed by the head office.Intervention programmes should be uniform across the country.You cannot just set a precedent and thus we were told to look into areas of support for the people,” he said.Under the programme, TB patients receive drought relief food to take with their medicine.He said the Ministry’s head office had told them that they were already burdened with the timely provision of medicine.”That is already enough a job,” he said.The diseases are the major causes of death people in the area face.Principal medical officer at the Keetmanshoop Hospital, Dr Emmanuel Dumebi Adigwe, said it was “just too difficult to control them”.In an interview with The Namibian, Adigwe said the issue was complicated by the dropout rate of those on TB treatment and the stigma that HIV-infected people face.”We are in pain over the defaulters.The dropout rate is worrying and the consequences are very harsh on the patients.They develop resistance,” he said.Statistics available from national TB campaigners indicate that the disease has not only became one of the two major causes of death but is responsible for a significant number of institutional deaths.When Namibia applied for funding from the Global Fund for AIDS, TB and Malaria, it indicated that 10 per cent of all deaths in Namibia were due to TB.Between 1991 and 2000, the rate of notification has risen from 430 for every 100 000 to 619/100 000 a year.The escalation is due to the link between the two diseases.Drug resistance has increased because some patients fail to follow prescribed schedules when taking their medicine.The Ministry has since introduced the Directly Observed Treatment, Short Course or DOTS strategy.Adigwe said defaulters were the most costly patients to treat and were spreading multi-drug resistant strains.Drug-resistant strains can cost up to N$25 000 to treat, as opposed to N$250 to treat a new infection.At best, only half of those infected with the new strains can be cured.If left untreated, one person can infect up to 15 others.The DOTS strategy relies on testing, monitoring and an uninterrupted supply of effective medicine.A person diagnosed with TB has to take medication every day for six months.For those who do not, TB can be deadly.Dr Adigwe said TB was worsened by the culture of sharing and the high rate of alcoholism in the region.”People drink at shebeens without eating.They tend to share one tombo container and if one has TB, it is likely to be spread.That is why Karas is one of the regions with the highest prevalence,” he said.Eventually, Dr Adigwe and his colleagues initiated a “food-for-TB” programme.”It was a local arrangement which was never blessed by the head office.Intervention programmes should be uniform across the country.You cannot just set a precedent and thus we were told to look into areas of support for the people,” he said.Under the programme, TB patients receive drought relief food to take with their medicine.He said the Ministry’s head office had told them that they were already burdened with the timely provision of medicine.”That is already enough a job,” he said.
Stay informed with The Namibian – your source for credible journalism. Get in-depth reporting and opinions for
only N$85 a month. Invest in journalism, invest in democracy –
Subscribe Now!